Legionellosis
Definition
- Infection caused by *Legionella* species (Legionella spp.)
Source of infection
- Legionella species
- Associated with aerosol-generating facilities such as cooling towers, building water systems (showers, faucets), humidifiers, respiratory therapy equipment, and hot springs
- Aerosols generated from household plumbing systems, grocery store misters, and natural or artificial hot springs
Transmission route
- Transmission occurs when bacteria in contaminated water (e.g., cooling tower water) from large buildings’ cooling towers, air conditioners, showers, intensive care respiratory equipment, faucets, decorative fountains, misters are dispersed as droplets and inhaled into the human body.
Common targets
- Pneumonic form (Legionellosis): Occurs frequently in individuals with chronic diseases, smokers, and immunocompromised patients.
- Influenza-like form (Pontiac fever): Attack rate over 90% during outbreaks, occurs frequently in individuals without underlying diseases.
Peak season
- Sporadic cases: Year-round
- Outbreaks: Summer to early autumn
Incubation period and contagious period
- Pneumonic form (Legionellosis): 2–10 days, average 7 days
- Influenza-like form (Pontiac fever): 24–48 hours, average 36 hours
- Human-to-human transmission: None reported
Clinical symptoms
- Pneumonic form (Legionellosis): Occurs frequently in individuals with with chronic lung disease, smokers, and immunocompromised patients.
- Fever, chills, dry cough or cough with a small amount of sputum, muscle pain, headache, general weakness, loss of appetite, gastrointestinal symptoms, impaired consciousness, etc.
- Chest X-ray: Pneumonia
- Complications: Lung abscess, empyema, respiratory failure, hypotension, shock, rhabdomyolysis, disseminated intravascular coagulation, renal failure, etc.
- Influenza-like form (Pontiac fever): Attack rate over 90% during outbreaks, occurs frequently in individuals without underlying diseases.
- An acute febrile illness lasting 2 to 5 days
- After the onset of symptoms such as fatigue and muscle pain, fever and chills occur, accompanied by dry cough, runny nose, sore throat, diarrhea, nausea, dizziness, etc.
Case fatality rate
- Pneumonic type (Legionellosis): Varies depending on susceptibility, but in hospitalized patients, 40–80%.
- Influenza-like form (Pontiac fever): No deaths.
Diagnosis/Reporting criteria
- Reporting scope: Patients, suspected cases
- (Patient) A person who shows clinical symptoms consistent with legionellosis and is confirmed to be infected with the infectious pathogen according to diagnostic criteria
- (Suspected case) A person suspected of having legionellosis based on clinical symptoms and epidemiological links, with infection presumed according to diagnostic criteria for a probable case
- Diagnostic criteria
- Confirmed diagnosis
- - Isolation and identification of Legionella bacteria from specimens (bronchial lavage fluid, bronchoalveolar fluid, bronchial aspirate, sputum, lung tissue, pleural fluid, blood, etc.)
- - Detection of specific antigen in specimen (urine), including rapid diagnostic kit
- - Antibody titer in convalescent serum increases more than fourfold compared to the acute phase.
- Presumptive diagnosis
- - Detection of specific antigen by direct immunofluorescence antibody test in specimens (bronchial lavage fluid, bronchoalveolar fluid, bronchial aspirate, sputum, lung tissue, pleural fluid, blood, etc.)
- - In specimen (blood), a single antibody titer of 1:128 or higher by indirect immunofluorescence antibody test
- - Detection of specific gene in specimens (bronchial lavage fluid, bronchoalveolar fluid, bronchial aspirate, sputum, lung tissue, pleural fluid, blood, etc.)
- Confirmed diagnosis
- Reporting period: Report within 24 hours
- Reporting method: Complete the notification form and report to the local public health center via web (http://eid.kdca.go.kr) entry or by fax.
- Responsible department: KDCA Division of Infectious Disease Control
Annual incidence rate of legionellosis
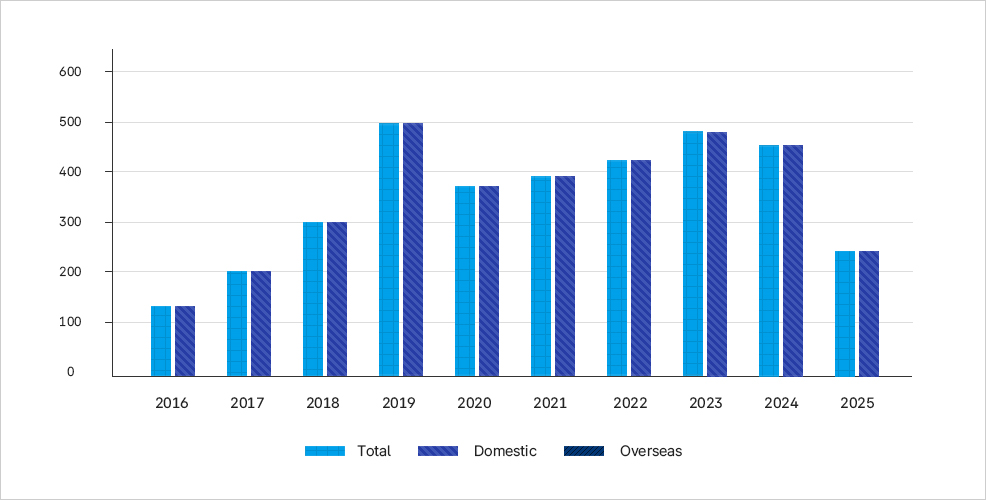
이 그래프는 2016년부터 2025년까지 연도별 레지오넬라증 발생률을 국내와 국외로 구분하여 보여준다. - 2016년 발생률은 약 130건 수준으로 비교적 낮았다. - 2017년에는 약 200건으로 증가했으며, 2018년에는 약 300건으로 더 상승했다. - 2019년에는 국내와 국외 모두 약 500건으로 정점을 기록하였다. - 2020년과 2021년에는 약 370~390건 수준으로 감소하였다. - 2022년에는 약 420건으로 다시 증가했고, 2023년에는 약 490건으로 2019년에 이어 두 번째로 높은 발생률을 보였다. - 2024년에는 약 450건 수준으로 소폭 감소했으며, 2025년 현재는 약 240건으로 크게 줄어든 상태다. 전체적으로 2016년 이후 발생률이 꾸준히 증가하다 2019년에 정점을 찍고, 코로나19 유행 시기인 2020~2021년에 다소 감소한 뒤 다시 증가하다 최근 2025년에 급감한 추세가 나타난다.
